In recent years, patient education has been the focus of extensive research in the field of pain rehabilitation. Education in a comprehensive rehabilitation program can reduce pain, and disability (1), reduce negative beliefs and perception about pain, catastrophizing, and kinesiophobia. (2)
This research emphasis matches patient expectations as most patients expect to be educated about their conditions and their management. They want information about the cause of their pain and underlying pathology and wish to have a legitimate/definitive diagnosis and diagnostic imaging. (1) They also want clear, trustworthy, and consistent information on prognosis, treatment options and self-management strategies that are tailored to their age, lifestyle, and occupation status. (1)
The debate that seems to be raging in the pain education science is what type of education benefits patients most. The two major types of education being often discussed in the literature are biomechanics/physiology and pain neuroscience. Pain neuroscience education (PNE) has been heralded to bring superior results compared to other forms of education. Recent studies cast doubts on this superiority. A just published randomized controlled trial by Adenis et al. showed no advantage of PNE over spinal physiology and ergonomics education. (2) An umbrella review on PNE in patients with chronic musculoskeletal pain published in 2023 reports no statistically significant improvement in terms of pain intensity, disability levels or psychosocial variables with the addition of PNE to other treatment modalities. (3)
Scientific studies can have methodological shortcomings that might affect patient outcomes and clinical recommendations, which can certainly be one explanation for the different results regarding pain education. What seems to be clear is that some form of education is helpful for patients. To be effective, educational interventions require to be targeted to the patients’ needs and expectations. The focus should then be shifted from figuring out which type of intervention is better to providing patient-centered care.
People play an active role in constructing and giving meaning to the world around them, including to the experience of pain. In this process, the mind is not merely a passive receptor of information, but an active participant in the creation of meaning and experience. (4) Many different dispositions (intrinsic and extrinsic contextual factors) will affect this sensemaking process. (5) The clinician roll then is to try to understand how patients give meaning to their experience by exploring these factors. Patient-centered care requires to include these elements in patients’ management.
Therapeutic alliance is a cornerstone of patient-centered care. Robust therapeutic alliance has been shown to improve patient outcomes. (5) (6) Therefore, clinicians need to implement strategies to bolster therapeutic alliance, emphasizing mutual connection, collaboration, and shared therapeutic objectives. (6) Approaches that can foster therapeutic alliance include active listening, bidirectional communication, understanding expectation, goal sharing, coordination, and adaptation. (6)
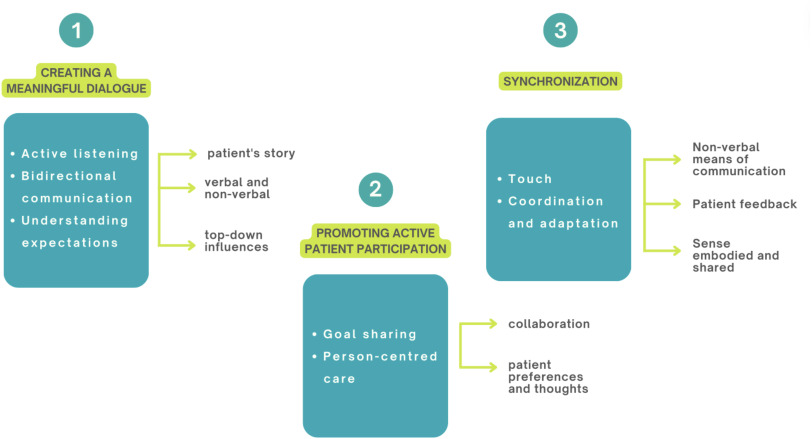
Effective patient-centered care requires the establishment of deep empathic connections and mutual communication to ensure a comprehensive exploration of the patient's problems. (6) Meaningful dialogue, active patient involvement and therapeutic synchrony strengthen therapeutic alliance (6) and patient outcomes. (5)
- Zadro, J.R. and Elkins, M.R. (2022) ‘Advice and education for spinal pain’, Journal of Physiotherapy, 68(2), pp. 86–88. doi:10.1016/j.jphys.2022.03.006.
- Adenis, N. et al. (2024) ‘Pain neuroscience education is not superior to spinal physiology and Ergonomics Education within a short multidisciplinary rehabilitation program: A randomized controlled trial’, Musculoskeletal Science and Practice, 74, p. 103176. doi:10.1016/j.msksp.2024.103176.
- Cuenca-Martínez, F. et al. (2023) ‘Pain neuroscience education in patients with chronic musculoskeletal pain: An umbrella review’, Frontiers in Neuroscience, 17. doi:10.3389/fnins.2023.1272068.
- Nesi, J., dos Santos, R.L. and Benites, M. (2024) ‘Exploring enactivism: A scoping review of its key concepts and theorical approach’, Advances in Integrative Medicine [Preprint]. doi:10.1016/j.aimed.2024.08.007.
- Vianin, M. Dispositionalism in Musculoskeletal Care: Understanding and Integrating Unique Characteristics of the Clinical Encounter to Optimize Patient Care. EVOLVE GLOBAL PUBLISHING. 2021
- Arrigoni, A. et al. (2024) ‘Exploring the role of Therapeutic Alliance and Biobehavioural Synchrony in musculoskeletal care: Insights from a qualitative study’, Musculoskeletal Science and Practice, 73, p. 103164. doi:10.1016/j.msksp.2024.103164.


