Multiple factors contribute to the experience of non-specific chronic low back pain, including structural and functional nervous system biomarkers, structural spinal tissue biomarkers spinal imaging, and psychosocial dispositions. Appropriate management of non-specific chronic low back pain requires the untangling of these factors by determining the importance of each element in the clinical presentation of the patient. Treatment strategies need to be targeted to the factors having the most impact on the patient.
A recent multivariate meta-analysis revealed that spinal imaging, psychosocial and nervous system biomarkers contribute to non-specific chronic low back pain. Interestingly, the effect size of the different contributors differ among factors. The largest effect size being reported for psychological factors.
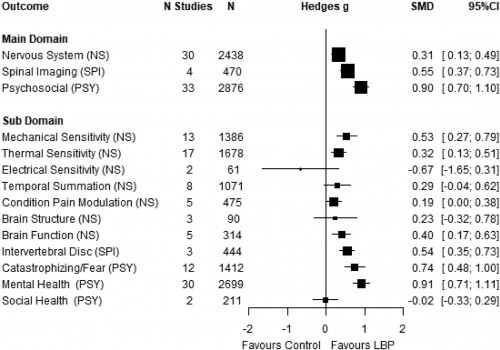
Specific factors such as catastrophizing and fear, depression and anxiety, pressure-pain thresholds, thermal pain thresholds and functional brain connectivity were significantly different in non-specific chronic low back pain compared to pain-free controls.
Psychosocial dispositions need to be screened on initial consult in patients with non-specific chronic low back pain using tools such as the STarT Back and Orebro Musculoskeletal Pain Questionnaire to determine their relative importance to the patient clinical picture and treatment consideration.


